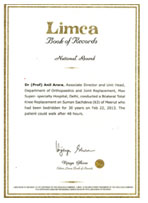
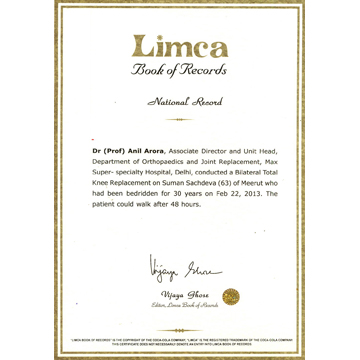
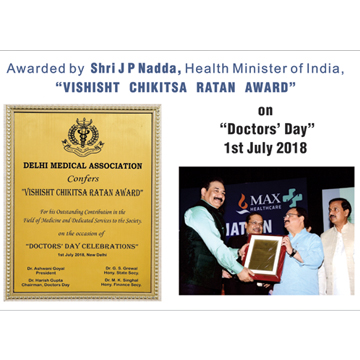
Prof. Anil Arora Guinness World Record Holder and Limca Book of Records Holder, is
considered as one of the Best Knee and Hip Replacement Surgeon, a Minimally Invasive,
Computer Navigated Advanced Knee and Hip Replacement Surgeon with experience of
more than 10,000 Joint Replacements!!! Being in this field from 1988, he has performed
countless (Advanced) Primary, Complex and Revision Knee and Hip joint replacement
operations. Patients reach to him not only from Delhi or National Capital Region of Delhi
(NCR) or from various part of India, but from overseas also including Non-Resident Indians
(NRI's).
Prof. Arora is one of the Best Joint Replacement Surgeon in Delhi, as he emphasizes on
RAPID RECOVERY PROTOCOLS to joint replacements, that remarkably reduces the recovery
time.
Prof. Arora applies team-based approach to ensure caring, compassionate, and holistic care
to all of his patients throughout their joint replacement journey. From pre-surgery
education, to compassionate bedside care, to supportive postoperative rehabilitation and
aftercare services, Prof. Arora and his team is with the patient every step of the way. He
emphasises on 24X7 availability of care, even after the patient is discharged from the
hospital, till full recovery.
Prof. Arora’s Knee & Hip Surgery Clinic's quality ratings are excellent; in particular the clinic is renowned for its exceptionally low rate of complications and high patient satisfaction scores. He performs around 1500 Joint replacement every year & that is why his Prof Arora’s Knee & Hip Surgery Clinic is considered one of the Best Knee and Hip Replacement Centre of India. When it comes to advanced joint replacements – experience & expertise matters.
Some of the Unique treatment modalities used by Dr (Prof.) Anil Arora are:
- ROBOTIC Joint Replacement
ROBOTIC Joint Replacement- It is the latest technology in the field joint replacement and is fast gaining popularity amongst patients and surgeons. In this type of surgeries, a significant part of the surgery is done by a robot under the supervision of a Joint Replacement Surgeon. ROBOTIC surgery is done with more precision, flexibility, and control than manual surgery. In the ROBOTIC technique, a live 3D model of the patient’s joint is created, which helps the surgeon to make a customized plan according to the patient's condition and requirement.
ROBOTIC Joint Replacement patients report better movements and have a very natural feel of the joint.
Read More
- PINLESS Computer Navigation System:
One of the Pioneers to start this technique in North India, this is the most recent
cutting-edge "PINLESS Computer Navigation System" which provides Computer
Navigated Knee Replacements with assured results. He is one of the Best Knee
Replacement Surgeons of India using this technology. Severe joint deformities can
also be addressed to perfection, using this technology.
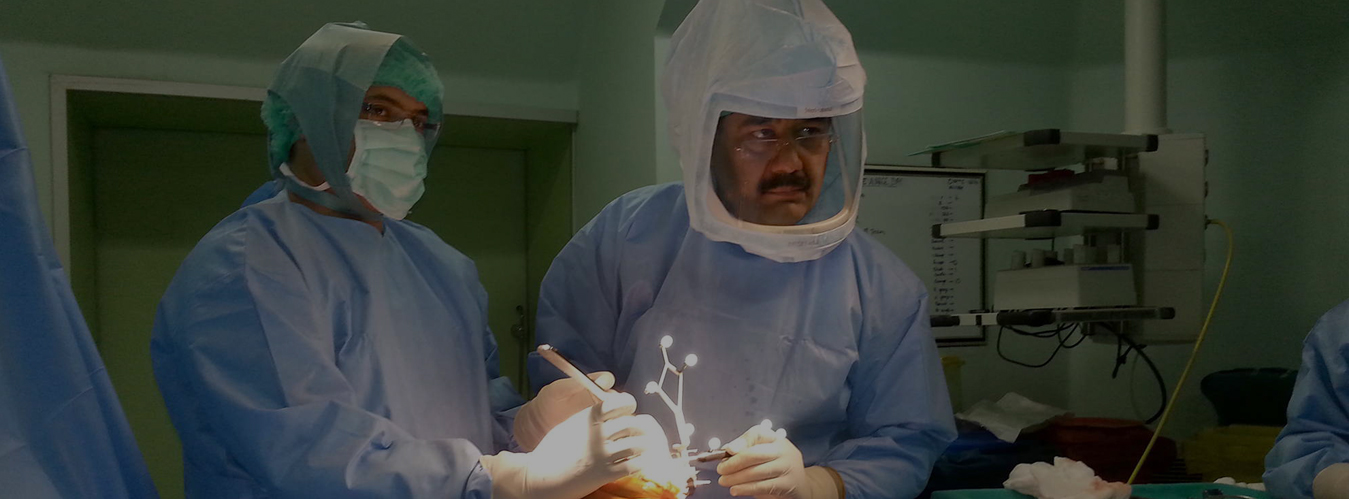
- Body Exhaust System
Body Exhaust System, the latest innovation in safe surgical practices to minimise
serious infections. Infection is considered as number one reason for early failure of a
joint replacement surgery. The technique involves wearing a body suit resembling an
Astronaut's Suit while performing surgery. This technique is specially recommended
for patients with diabetes & all those who are prone for infection.
Prof. Arora is a name to reckon with when it comes to joint replacement. His clinical
acumen, surgical skills & humane practice sets him apart. His team is committed to patient
care & ensures every patient is looked after well during & after the course of treatment. He
believes in patient education & communication. His team is available 24 X 7 to address each
and every query or concern of the patient. No wonder he is considered one of the Best Knee
and Hip replacement Surgeon of Delhi.